A lot of arguments don’t end because someone “lost.” They end because someone drops a category word: harmful, hateful, unsafe. The conversation gets reclassified as an emergency, and suddenly you are no longer debating a claim. You are defending your right to be in the room.
If you’ve felt this happening more often lately, you’re not imagining it. The move is simple: treat disagreement as injury, then treat your refusal to retract as more injury. It’s a neat little loop. You can’t disprove it, because your attempt to disprove it is counted as part of the harm.
So the goal here isn’t to “win” every exchange. The goal is to stay clear, stay calm, and avoid being dragged into fog.
Three rules help.
1) Ask what the harm is, mechanically
“Harm” is a suitcase word. People pack a dozen meanings into it, then wheel it around as if it’s one thing.
Don’t fight the suitcase. Open it.
Try:
-
“What kind of harm do you mean: emotional distress, social exclusion, incitement, discrimination, or something else?”
-
“What’s the actual path from my claim to the harm you’re naming?”
-
“Is the harm that you dislike the idea, or that you think it leads to a specific outcome?”
This isn’t a gotcha. It’s basic hygiene. If a person can’t tell you what they mean, you cannot respond intelligently. You’re shadowboxing.
A good rule of thumb: if they can’t name a mechanism, they aren’t making an argument. They’re placing a stop sign on the table and acting like the sign is evidence.
And notice the comfort “harm” provides. It allows someone to skip the hard part, the part where they explain why your claim is false, or why it leads to a concrete bad result. They can just announce: “That’s harmful,” and then expect you to retreat on cue.
Make them do the work. Not as punishment, but because without that work you are not in a debate. You are in a moral weather report.
2) Separate moral judgment from permission to censor
Even if a statement is rude, wrong, or ignorant, it does not automatically follow that it should be suppressed or punished.
That leap is the whole game.
You’ll notice how quickly some conversations smuggle in this assumption: if it’s harmful, it must be disallowed. But that premise is not neutral. It’s political. It’s also the premise that makes “harm” such a powerful word, because it offers a shortcut from “I condemn that” to “you don’t get to say that.”
Break the spell with a calm distinction:
-
“You’re free to think I’m wrong. That doesn’t mean you’re entitled to make me silent.”
Or softer:
-
“We can disagree strongly and still protect the right to say it.”
This forces a choice. Are they arguing that you are mistaken, or are they arguing that mistaken speech is illegitimate?
In a plural society, we tolerate a lot of speech precisely because we do not trust any faction, left or right, religious or secular, activist or corporate, to define “harm” without expanding it until it covers whatever irritates them this week.
Also: don’t let “consequences” do lazy work. Yes, speech can have consequences. So can silence. So can mandatory agreement. So can the habit of treating adults like fragile glassware.
You can live in a world where people criticize each other sharply. That’s normal. What you cannot do, without slowly breaking civic life, is turn moral condemnation into a veto.
Criticism is fair game. Coercion is not.
3) Don’t get trapped in intent court
When someone says “That’s hateful,” they often mean: “Your intent must be hateful.”
Now you’re in a trial about your inner motives, which is the safest place for them. It’s unfalsifiable. You can’t prove you don’t hate. They can’t prove you do. But they can keep you stuck there forever while the original claim remains untouched.
So: state your intent once, briefly, then return to the claim.
A template that works:
-
“My intent isn’t to attack anyone. The claim is X. If X is wrong, show me where.”
That’s it. One sentence of intent, then substance.
If they refuse and keep circling back to your hidden motives, set a boundary:
-
“If your position is that disagreement equals hate by definition, then there isn’t a debate to have.”
This is not escalation. It’s diagnosis. Because at that point the argument is no longer about facts, reasons, or tradeoffs. It’s about social control: the category word has been used to declare you out of bounds, and your only permitted move is submission.
The point of the exercise
The goal isn’t to dunk on people. It’s to keep the conversation from being hijacked by fog words and moral shortcuts.
So:
-
Define the harm (mechanism, not mood).
-
Separate judgment from censorship (criticism isn’t a veto).
-
Refuse the intent trap (claims, not soul-reading).
If they can engage those terms, you might actually have a discussion. If they can’t, you’ve learned something useful. You learned it without flailing, apologizing for existing, or agreeing to a vocabulary designed to make debate impossible.
And that, in 2026, is already a small victory.


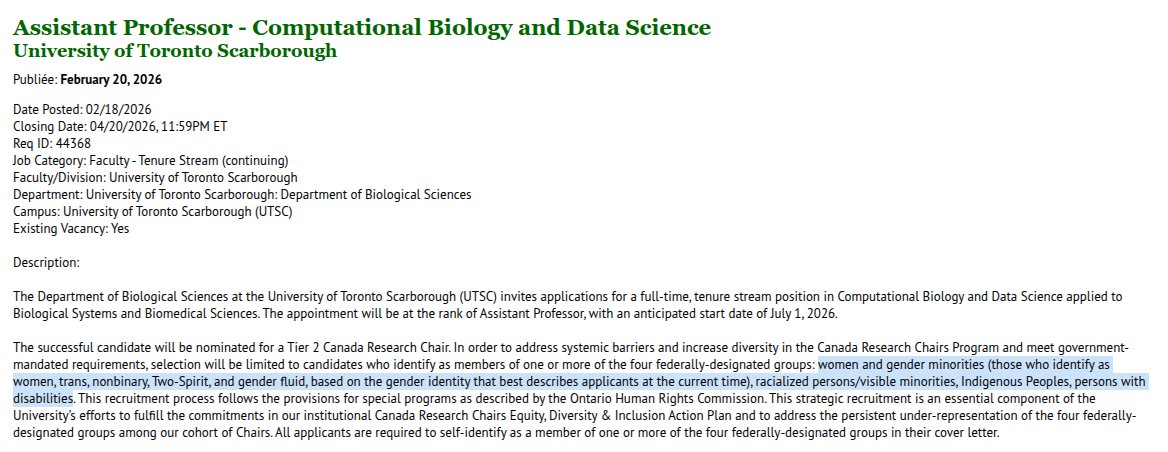 The posting requires applicants to self-identify as a member of one or more “designated groups” in their cover letter, namely women or gender minorities, racialized persons, Indigenous Peoples, or persons with disabilities. If you do not fit one of those categories, you are not eligible to apply. That is not an inference. It is in the posting.
The posting requires applicants to self-identify as a member of one or more “designated groups” in their cover letter, namely women or gender minorities, racialized persons, Indigenous Peoples, or persons with disabilities. If you do not fit one of those categories, you are not eligible to apply. That is not an inference. It is in the posting.




Your opinions…